Preventing Dental Implant Failures
Good Oral Hygiene and
Clinician Expertise Matters

What Causes Dental Implants to Fail?
Dental implants can restore more than 99% of natural function, enabling you to eat all the foods you love, as well as smile, talk and laugh without feeling self-conscious. Although dental implants have a high success rate of 95–98%, several factors can cause dental implant failure.
Inadequate fusion with the underlying bone and a progressive inflammatory disease called peri-implantitis are the primary reasons implants fail. Both are closely associated with poor oral hygiene and untreated periodontal disease. Smoking has been shown to restrict blood flow and interfere with surgical healing, thereby significantly increasing the risk of dental implant failure.
A 2021 study concluded that smokers have a 140.2% higher risk of failure than implants placed in non-smokers. If you have active gum disease, this must be treated prior to placing dental implants to ensure proper fusion with your jawbone. In addition, getting inferior implants from a clinician without extensive surgical experience can lead to failure.
At Rain Dental Implant Centers, our skilled oral surgeons have vast experience assessing whether patients are ideal candidates for dental implants and providing preliminary treatments that reduce the risk of complications and help increase the likelihood of long-term success.

Dr. Brooks Talks About The Role That Technology Plays In Dental Implant Placement
Dental Implant Failure Risk Factors
The long-term survival rate of dental implants is well documented. With that said, multiple studies have shown that thorough clinical and radiographic pre-surgical evaluation of a patient’s bone quality and quantity is imperative for successful implant treatment.
Even patients with advanced bone loss with less than favorable prognoses treated by clinicians with extensive expertise in initial surgical and supportive therapy have high long-term success rates. These patients may also be cccandidates for zygomatic dental implants, specialized longer implants that are placed in the zygomatic (cheek) bone.
In addition, studies indicate patients who adhere to strict hygiene visits combined with diligent home care can prevent the progression of gum disease and achieve long-term success.


Issues Associated With An Increased Failing Implants
- Diabetes
- Immune system disorders
- Steroid therapy, chemotherapy or radiosurgery
- Excessive bruxism (tooth clenching/grinding)
- Cigarettes, cigars and smokeless tobacco use
- Implant malposition
- Previous implant failure
Are You A Candidate For Dental Implants?

What is Peri-Implantitis?
As with untreated gum disease in which infection can impact a natural tooth root, bacteria that forms around an implant can lead to a serious infection. The difference is that the inflammatory process is more intense and progresses quickly compared to inflammation around natural teeth.
While the exact incidence of peri-implantitis is unknown, various studies suggest 5–8% of dental implants are affected by this condition. Early symptoms include swollen gums, tenderness and sensitivity in the mouth.
The earliest stage of peri-implant disease is called peri-implant mucositis. Gum inflammation is limited to the soft tissues around the dental implant, with no signs of bone loss. Evidence suggests peri-implant mucositis can be successfully treated and reversed with early intervention. When the disease progresses to peri-implantitis, jaw pain may increase, the gum line can recede, gum pockets deepen, the implant threads may become exposed, pus may develop around implants and they can loosen.
When left untreated, the most severe cases of peri-implantitis require removal of the implant and bone grafting to replace the damaged bone.

How is Peri-Implantitis Treated?
Peri-implantitis treatment can be accomplished with a dental laser or traditional surgery using a scalpel. The goal of both is to eliminate the infection around the implant and treat the underlying causes impacting the health of the bone and implant. With laser treatment, a fiber the width of three human hairs is inserted between the implant and the gum. Laser energy kills the bacteria, vaporizes cement and stimulates stem cells found in the bone to reduce the infection and promote healing. With a scalpel, the gum tissue is cut and flapped back, the implant is cleaned and foreign materials may be placed in the area to help promote bone growth. Then the tissue is sewn back together.


Postsurgical Tips to Prevent Implant Failure
To reduce the risk of infection, you need to take the prescribed oral antibiotic and use the antibacterial rinse we provide. We’ll also discuss dietary guidelines that you need to follow to prevent complications. This includes drinking plenty of fluids, avoiding hot liquids or very warm foods and progressing to soft foods after being able to tolerate liquids. Warm salt water rinses should be used at least four to five times a day, especially after meals. We recommend refraining from smoking until the implants have fully integrated with your underlying bone.

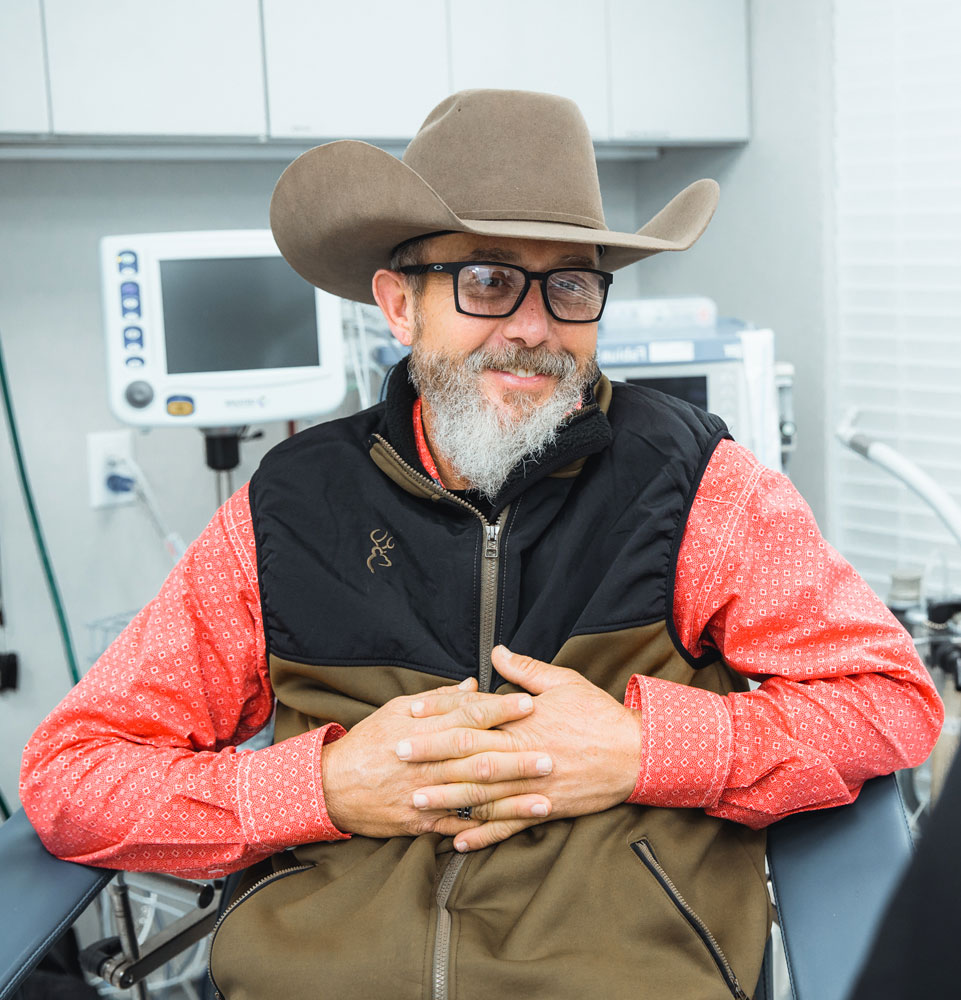
Dr. Jensen Talks About Why Experience Matters When It Comes To Dental Implants
Selecting the Right Clinician
Helps Ensure Successful Outcomes
Dental implants are the number one tooth replacement due to their unsurpassed strength, longevity, and natural-looking aesthetics, yet the decision to replace missing teeth shouldn’t be taken lightly. Choosing a state-if-the-art dental implant center with a long and proven track record will significantly reduce the risk of failure and ensure the best outcomes.
When you get dental implants at Rain Dental Implant Centers, rest assured your smile will be in some of the most capable and experienced oral surgery hands in the U.S.
